Ten Things I’ve Learned About Doctors, Diagnosis, and Getting Help When You're Chronically Ill.
- Genevieve Hawtree
- Jul 13
- 6 min read
Updated: Jul 15
After more than five years of living with chronic illness - including chronic migraines, neurological symptoms, fatigue, and widespread pain - I’ve seen my fair share of doctors and medical professionals. Here are some things I have learned....
1. Doctors don’t know everything.

Before I got sick, I believed what a lot of people do - that if something were seriously wrong, a doctor would know what it was and how to fix it. We’ve all seen it on Greys Anatomy, right? Doctors racing to solve the mystery and save the day. But in real life, most doctors have 10 minutes - 20 if you’re lucky - to make their best guess.
Medicine moves fast, and no one doctor can keep up with everything - especially rare stuff. So just because your doctor doesn't have an answer for you - it doesn't mean the answer isn't out there. And spoiler: no one's running labs like it's an episode of House. You’re lucky if they remember what you said last time.
2. Doctors are human - and they get tired.
On an average day, a doctor might see dozens of patients. They’re busy, they’re exhausted, and sometimes they don’t give each appointment the thought it deserves. They rely on pattern recognition and quick judgments, which means you might get the fastest answer - not the most accurate one. This means sometimes they will be wrong. Knowing that is important especially for those of us who were taught to believe what our doctors tell us.
3. Bias exists in medicine.
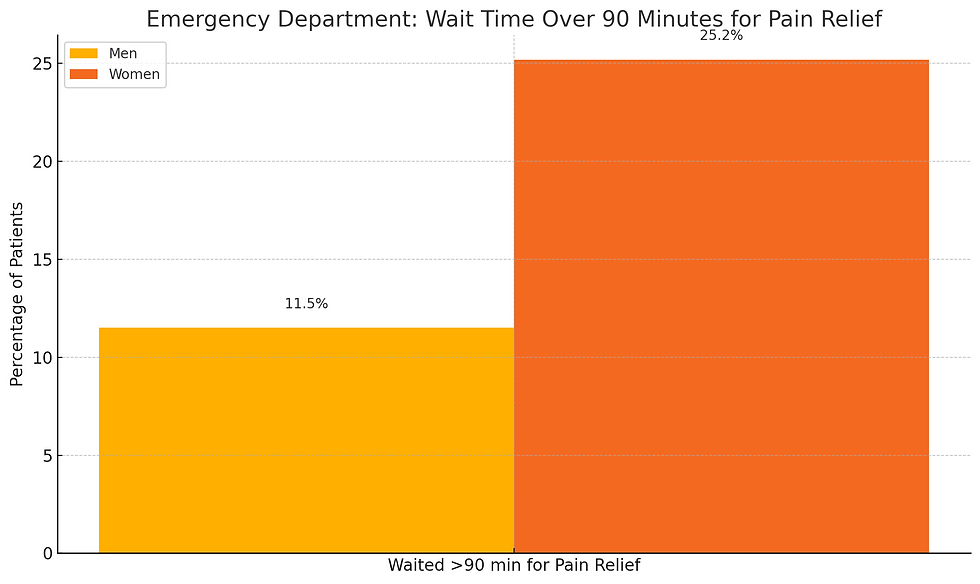
Research backs up what many of us have lived: men are more likely to be believed, while women and people of colour are often dismissed or misdiagnosed. And it doesn’t stop there - other forms of bias show up too, like ageism, weight bias, and ableism. People who are overweight, older adults, and disabled patients are all less likely to receive proper treatment for pain and more likely to be told it’s psychological.
I’m a bigger woman and always have been. I can tell the moment a doctor decides my weight is the cause of everything. It’s not subtle—it’s the quick pivot to diet talk when I came in for dizziness and neurological symptoms, or the suggestion to exercise more when I’m telling them about my migraine pain. Once that switch flips, it’s hard to bring the conversation back to what I actually need help with.
It’s exhausting, but recognizing bias helps. It helps you push back, ask better questions, and advocate for yourself—even if you shouldn’t have to.
4. You have to do your own research.
When doctors keep coming back with a diagnosis of anxiety-and you’re being told to lose or gain weight, exercise more, and "not worry about it"-sometimes you need to do a little digging for yourself. Researching your symptoms and finding conditions that match can be both validating and helpful in moving toward a proper diagnosis. Visiting official websites for illnesses that seem to fit can lead you to useful tools and suggestions for navigating the system and helping yourself.
That said, be careful. Not everything online is helpful or trustworthy. Good sources explain where they got their information, avoid miracle promises, and back things up with real evidence. There are a lot of people out there claiming to have the solution to your problems-for the low, low price of $19.99. Be cautious.
Sometimes it really does feel like you need a medical degree just to get help—I know I feel like that sometimes. But what you’re actually doing is building a better understanding of the possibilities and giving yourself the tools to ask smarter questions about your health.
5. You need to learn how to manage egos.
Doctors don’t always like being told they’re wrong. Many feel pressure to have all the answers, and it can make them defensive. That means learning to communicate in ways that give your doctor room to reconsider without feeling threatened.
Share your observations as a question. Point to resources gently by asking what your doctor thinks about something you’ve read. Give them the opportunity to come back more informed. And remember - sometimes diplomacy works better than confrontation.
It shouldn’t be your job to protect someone else’s ego when you're unwell - but sometimes, finding a path through that dynamic is the only way to get what you need. You’d think after 10 years of med school they could handle a little curiosity - but hey, here we are.
6. It might take multiple visits to get answers.
A single appointment might not be enough for your doctor to understand the full picture. You may need to keep going back, repeating yourself, building trust, and being persistent to get the care you need.
It’s exhausting. It can be demoralizing. But sometimes, persistence is what gets you taken seriously. In the last year I have seen my neurologist 4 times, my doctor 10 times and other specialists 3 times. It is just part of the process.
7. Preparation makes a huge difference.
I used to show up to appointments and just try to wing it. I’d forget what I wanted to say or leave out something important. Now, I make a cheat sheet before every single appointment. It includes my diagnoses (both confirmed and suspected), a list of symptoms grouped by type (neurological, muscular, etc.), my medications, and any questions I want to ask. I hand it to the doctor so I know I haven’t forgotten anything - and so they have something to look at later. This helps both of us get more quickly to the point of the appointment avoid repetition and get closer to answers.
8. You’ll probably try a lot of things that don’t work.
Even with all your prep and research, sometimes your doctor will suggest something that doesn’t help. Or worse-it makes things worse. But if you want them to stay engaged, you might have to try what they suggest-unless it’s clearly a no-go for your body or history. Sometimes you have to jump through hoops just to prove you’re willing to try.
That said, it’s also okay to say no. You have every right to ask questions, set limits, and take your time. But here’s the hard truth: if you flat-out refuse a treatment because you think you already know what’s wrong, you may be seen as “difficult” or “non-compliant” and that can work against you. You might also miss out on something that could help.
I once had a doctor prescribe me anxiety medication. I don’t have anxiety, and I was pretty sure it wouldn’t help. But I gave it a shot-and it didn’t fix anything major, but it did help me sleep better. So, bonus! I’ve tried 14 different medications for migraines. Fourteen. Trial and error is sometimes part of the game. It is frustrating, yes, but occasionally something surprising works.
That’s why it’s so important to keep track of what you’ve tried, what helped, what didn’t, and what caused side effects. That log becomes part of your toolkit. Even failed attempts give you (and your doctor) more information to work with.
9. Negative tests don’t mean you’re not sick.
There are plenty of chronic illnesses that don’t show up clearly on lab tests or scans. A “normal” result doesn’t mean you’re fine. It doesn’t mean it’s all in your head. Sometimes a diagnosis only comes after everything else has been ruled out-and that process can take years.
Conditions like ME/CFS, fibromyalgia, migraines, endometriosis, hEDS, POTS, and MCAS are all real, life-altering conditions that often don’t show up on standard blood work or imaging. You can feel exhausted, dizzy, in pain, or completely off-and still be told your results are “within normal range.”
If you feel awful but your tests are normal... you might just need to keep looking. Normal test results don’t mean you’re imagining things. They just mean the tools being used aren’t catching what’s going on. Keep tracking, keep asking questions, and if you can-keep pushing for answers.
10. Your body is talking to you – take notes.
Your body is always sending signals. Pain, fatigue, brain fog, weird sensations—they’re all ways your body says, “Something’s not right.” It’s the same system that tells you when something is too hot or too cold- it’s also how your body tells you it’s not well.
And yes, you have to listen, even when other people can’t see what’s going on. One of the best ways to do that is to write it down. Keeping a symptom log helps you spot patterns-what’s making things worse, what’s helping, what’s changing. Many conditions (like migraines) can only be diagnosed once a log has been kept.
It’s not just busywork. It’s information about you and it is proof. For your doctor, and for you. It might be one of the most important things you can do to help you find answers.
So there you have it ... ten things I’ve learned (so far) on this medical journey. I hope something here helps you feel a little more seen or a little more prepared. What would you add to the list? What’s your experience been like with the medical system?








Comments